Dysembryoplastic Neuroepithelial Tumor
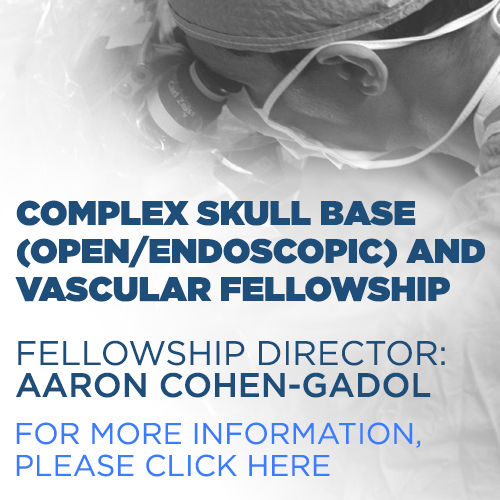
Figure 1: The dysembryoplastic neuroepithelial tumor (DNET) in this patient's lateral right temporal lobe is visible as involving the cortex and white matter. (Top Left and Top Right) There is typical bubbly cystic changes throughout the lesion visible on T2WI and FLAIR. The lesion is fairly circumscribed and demonstrates adjacent cortical thickening/dysplasia. (Bottom Left) Low-signal-intensity facilitated diffusion on DWI indicates a very low-cellularity watery tumor. (Bottom Right) No enhancement is present on T1-weighted postcontrast image.
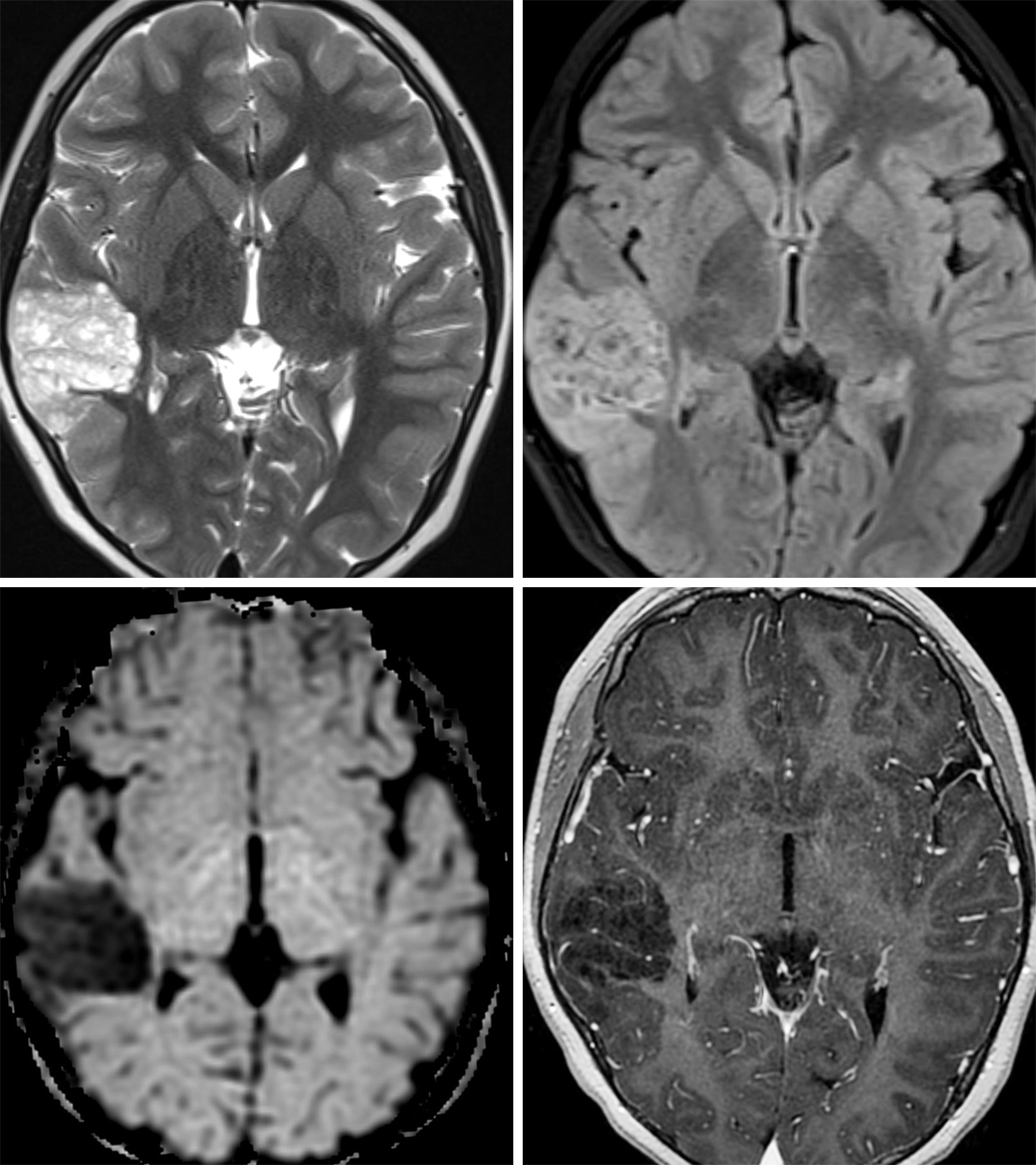
Figure 2: This DNET demonstrates bright T2 signal intensity (top left) that partially suppresses on FLAIR (top right), implying a watery tumor. The lesion is very superficial, involving cortex and white matter. The typical bubbly cystic changes are absent in this lesion, making diagnosis somewhat less specific. (Bottom) Like the majority of DNETs, this lesion has no enhancement on postcontrast imaging.
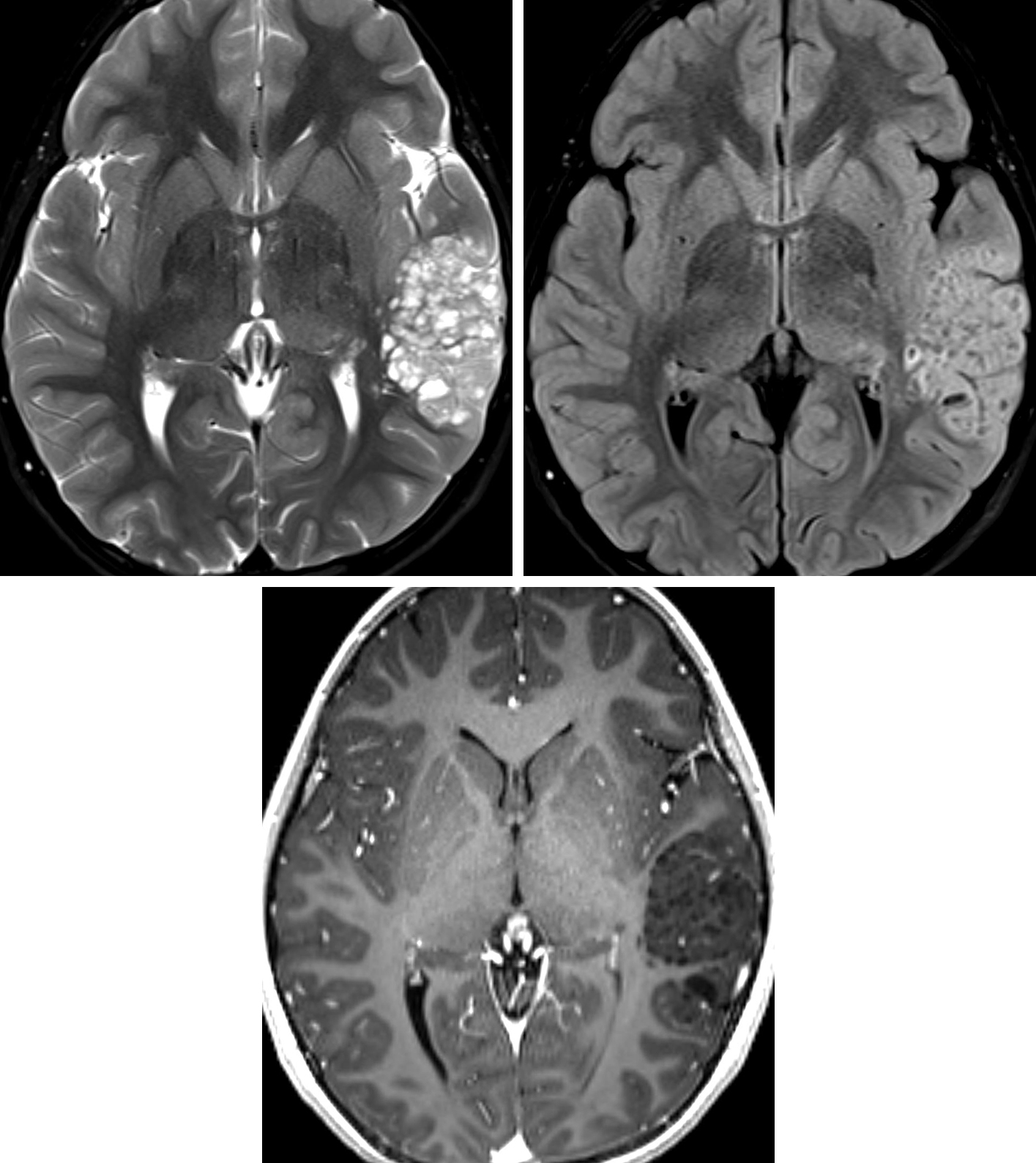
Figure 3: This 7-year-old girl demonstrates a large cystic “bubbly” DNET in the left temporal lobe. The T2 hyperintense cystic components (top left) demonstrate suppression of the fluid component on FLAIR (top right), while the remainder solid component of the lesion remains mildly hyperintense. (Bottom) No contrast enhancement is present within the lesion, typical for DNETs.
BASIC DESCRIPTION
- Benign, slow-growing neuroglial tumor
PATHOLOGY
- WHO grade I
- Likely arising from germinal matrix and extending along neuronal migratory pathway to cortex
- “Specific glioneuronal element” is characteristic feature
- Bundles of axons oriented perpendicular to cortex
- Viscous cystic components filled with neuroglial material
- Commonly shows calcification
CLINICAL FEATURES
- Commonly presents in second and third decades of life
- Slight male gender predilection
- Commonly presents as drug-resistant epilepsy/partial complex seizures
- Usually sporadic; rare association with neurofibromatosis type 1 (NF-1)
- Treatment: surgical resection
- Prognosis: favorable with complete surgical resection, complete resolution of seizures after surgery is common
IMAGING FEATURES
- General
- Well-defined, intracortical, wedge-shaped mass; often pointed toward ventricle
- Cystic or bubbly appearance
- Temporal > frontal lobe
- May show calcification
- Associated with cortical dysplasia
- CT
- Wedge-shaped cortical and subcortical hypodense region, can mimic ischemic stroke
- ±Scalloping of inner cortex, calcification
- MRI
- T1WI: lobulated, bubbly hypointense mass
- T2WI: usually hyperintense bubbly appearance
- FLAIR: variable signal, lacks adjacent edema
- T1WI+C: usually nonenhancing
- DWI: no restricted diffusion
IMAGING RECOMMENDATIONS
- http://doi.org/10.1007/s00381-015-2675-9MRI with contrast
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Bilginer B, Yalnızoglu D, Soylemezoglu F, et al. Surgery for epilepsy in children with dysembryoplastic neuroepithelial tumor: clinical spectrum, seizure outcome, neuroradiology, and pathology. Childs Nerv Syst 2009;25:485–491. doi.org/10.1007/s00381-008-0762-x.
Bulakbasi N, Kocaoglu M, Sanal TH, et al. Dysembryoplastic neuroepithelial tumors: proton MR spectroscopy, diffusion and perfusion characteristics. Neuroradiology 2007;49:805–812. doi.org/10.1007/s00234-007-0263-8.
Grossman RI, Yousem DM. Neuroradiology, The Requisites. Mosby, Maryland Heights, MO; 2003.
Osborn AG, Salzman KL, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Ranger A, Diosy D. Seizures in children with dysembryoplastic neuroepithelial tumors of the brain—a review of surgical outcomes across several studies. Childs Nerv Syst 2015;31:847–855. doi.org/10.1007/s00381-015-2675-9.
Please login to post a comment.