Management of Intraoperative Rupture
This is a preview. Check to see if you have access to the full video. Check access
Intraoperative Rupture of an MCA Aneurysm during Exposure (Pre-Dissection phase) without Proximal Control
With advances in endovascular therapy for intracranial aneurysms, patients with increasingly complex aneurysms are being referred for microsurgical procedures. As a result, the skills and outcomes of the neurovascular surgeon are under close scrutiny.
One of the most dramatic and potentially devastating complications during aneurysm microsurgery is intraoperative rupture (IOR). Containment of IOR and its sequel can make important contributions to minimizing complications from microsurgery. The incidence of IOR has been reported in 7% to 35% of cases. Several factors are associated with IOR: the surgeon’s experience, aneurysm size and morphology, and history of rupture.
Notably, the effect of IOR on patient outcomes is not well understood. Some series show no differences in outcomes, whereas others demonstrate poorer outcomes in patients who experience IOR. Batjer and Samson reported an 88% favorable outcome in patients without IOR, which decreased to 62% in patients with IOR. In a review of the Cerebral Aneurysm Rerupture After treatment (CARAT) study, periprocedural death and disability increased from 18% to 31% in patients who experienced IOR.
Intraoperative rupture during surgery bears some similarities and some major differences from intraprocedural rupture during endovascular treatment. The rates of intraprocedural rupture are significantly lower for endovascular therapy, with studies estimating an incidence of 1% to 9%. Management of IOR, however, may be more difficult through endovascular routes.
The CARAT study reported a 64% rate of death and disability in patients experiencing an intraprocedural rupture during endovascular treatment, more than double the rate for microsurgery. This increased risk of poor outcomes makes logical sense because bleeding often cannot be quickly controlled and decompressed during endovascular procedures as it can during microsurgery.
Intraoperative rupture is potentially avoidable, but nonetheless it will occur in some cases, and must be managed successfully to achieve good results. IOR can occur at several distinct time points during surgery. Steps to avoid and deal with it depend on the stage of the operation or phase of dissection, and aneurysm location and configuration. The point at which the complication occurs dictates the management options available.
IOR During Exposure
Although the occurrence of an aneurysm rupture during exposure is uncommon and associated with less than 10% of all IORs, the outcomes from this event can be catastrophic. During this stage of surgery, the surgeon has not yet had an opportunity to identify the anatomy of the relevant vasculature and the aneurysm, and in some cases, has not even begun microdissection.
This early stage of surgery commences from the moment the patient enters the operating room to the onset of vascular microdissection. There are numerous potential causes of rerupture during this time. Inadequate anesthesia during intubation and pin placement can lead to wide variations in blood pressure, leading to IOR.
The surgeon should exercise care during bone removal. Excessive use of the drill, especially during removal of the lesser sphenoid wing, can transmit vibrations to the aneurysm dome, precipitating rupture. Finally, excessive drainage of cerebrospinal fluid (CSF) may change the transmural pressure of the aneurysm, leading to destabilization of its wall.
Aggressive early retraction on the lobe attached to the dome of the aneurysm should be avoided. Specifically, in the case of posterior communicating artery (PCoA) and anterior choroidal artery aneurysms, early retraction on the medial temporal lobe may lead to IOR by placing traction on the aneurysm dome. Middle cerebral artery (MCA) aneurysms often point laterally and are attached to the surface of the temporal lobe, and therefore gentle and dynamic frontal lobe mobilization using the suction apparatus is a safe strategy to expose the proximal aneurysm neck and the M2 branches before temporal lobe retraction is contemplated.
Please see the first video at the beginning of this chapter for further details.
In patients with sizable hematomas, such as an MCA aneurysm with a frontotemporal clot, care must be taken when decompressing the hematoma. Excessive removal of the clot can destabilize the aneurysm sac, leading to rupture. If too little clot is removed, the surgeon may have to excessively retract the aneurysm-bearing lobe, and this maneuver can also destabilize the aneurysm.
Unfortunately, there are a limited number of options available to the surgeon if rupture occurs before exposure of the aneurysm or proximal control. In these instances, the surgeon must reduce the hemorrhage and clear the surgical field to allow rapid dissection of the dominant parent feeding artery or the aneurysm. This can sometimes be accomplished by using a large bore suction to follow the hemorrhage to its source.
The intravenous administration of adenosine can be dramatic and life saving by providing temporary cardiac arrest, although this maneuver often provides only 30 to 60 seconds of relief. Profound lowering of the blood pressure may place the patient at high risk for cerebral infarction. If the aneurysm is on the anterior circulation, cervical carotid compression may slow bleeding and allow some control over the hemorrhage.
Ultimately, the surgeon’s goal is to gain proximal vascular control by placing a temporary clip on the proximal arterial supply to the aneurysm. This will provide cessation of torrential hemorrhage to allow microdissection of the aneurysm neck and clip application. Brain protection with burst suppression using propofol or barbiturates may be useful. Rapid closure with no attempt to find proximal control with the hope of intracranial tension tamponading the bleeding is not recommended and will likely result in a poor outcome.
If the surgeon can follow the jet of blood to its source, he or she may control bleeding by placing a loose cotton ball over the bleeding site of the aneurysm sac. A self-retaining retractor can then be gently placed on the cotton to tamponade the bleeding and free up the surgeon’s hands to definitively deal with the aneurysm.
The surgeon must take care not to exert too much retractor pressure on the aneurysm as this could worsen the tear. Alternatively, a temporary clip may be “blindly” placed around the group of proximal arteries to briefly control overwhelming bleeding.
IOR during Dissection without Proximal Control
Rupture of an aneurysm prior to microdissection or during exposure, as described above, is associated with many factors outside the immediate control of the neurosurgeon. When an aneurysm ruptures during dissection, the complication is likely caused by a problematic operative maneuver performed by the surgeon. Fortunately, at this stage of the operation, there are more options available that allow for improved outcomes when compared with IOR during exposure.
The most likely cause for IOR at this stage is the operator’s incomplete understanding of the relevant vascular anatomy, namely the location of the aneurysm dome, neck, and important arterial branches. Wide opening of the Sylvian fissure by sharp dissection through a frontotemporal approach exposes most anterior circulation aneurysms safely, drains CSF from the cisterns, relaxes the brain, minimizes the risk of IOR, and reduces or eliminates the need for fixed retractors.
Most IOR’s occur because of indiscriminately aggressive blunt as opposed to sharp dissection techniques. Sharp dissection is one of the hallmarks of microsurgery to minimize complications. Gentle blunt dissection using fine dissectors is safe as long as this maneuver is performed for delicate arachnoid layers and minimally adherent vascular walls.
Management options of IOR at this stage of surgery require skill and decisive operative measures. Good outcomes are possible if the surgeon remains calm, stays in control, and executes calculated and deliberate maneuvers. In my opinion, the operator’s thoughtful technical reactions, rather than the IOR, are the most important determinants of final outcome.
The first step is to use two large bore suctions to clear the field and identify the site of the hemorrhage. If the relevant vascular anatomy is not sufficiently exposed, I use the suction tip to follow the flow of blood to the aneurysm. Next, I obtain reasonable control over the torrential bleeding by placing a small piece of cotton on the point of bleeding and use the suction tip and apply gentle tamponade.
With suction controlling the hemorrhage at the exact site of bleeding, I can often complete some dissection of the vascular tree for either temporary clip placement on the feeding vessel or rarely tentative clip ligation of the aneurysm/bleeding site. If the surgeon requires bimanual dissection to finish preparation of the vasculature, a fixed retractor blade can be placed carefully over the cotton on the rupture site to tamponade the aneurysm. In some cases, the surgeon can tentatively clip the rupture site on the aneurysm dome and later revise the clip location for complete neck obliteration when dissection is complete.
Most importantly, the surgeon must avoid rushing to blindly clip the aneurysm because this maneuver can worsen the tear in the dome or avulse the surrounding perforators. I advise the use of local circulatory arrest with proximal and distal temporary occlusion to identify the exact angioarchitecture of the aneurysm, the parent vessel, and important neighboring perforators.
If temporary clipping is possible, hypotension must be avoided and a cerebral protectant such as etomidate should be used. If temporary clips cannot be used, transient cardiac arrest with intravenous adenosine should be strongly considered. If the operator panics, it invariably leads to disappointing decisions and poor outcomes.
Intraoperative Rupture of an MCA Aneurysm without Proximal Control
IOR after Securing Proximal Control
The methods to control IOR are related to the specific cause during this phase.
IOR during Pre-Clip Application
During final dissection, but before clip application, the causes of IOR are generally related to blunt dissection. If the surgeon avoids early temporary clipping when necessary, he or she may fight the turgid aneurysm. This “fight” often leads to IOR. I have a low threshold for using temporary proximal clip ligation for short periods of time (less than 5 minutes) to enhance the safety of effective clip application while conducting high-risk maneuvers. Two minutes of reperfusion is allowed in between these periods of temporary occlusion.
Aneurysm relaxation can then be confirmed by gently “nudging” the aneurysm wall with the suction tip. If the aneurysm does not soften with placement of the clip, the operator should reexamine the temporary clip blades to ensure their circumferential location across the feeding vessel or look for incomplete clip blade closure caused by the presence of atherosclerosis in the wall of the corresponding vessel. Additional temporary clips ensure complete collapse of the walls; however, temporary occlusion of an atheromatous internal carotid artery may be impossible or unsafe.
At this stage, IOR may also be directly attributed to the surgeon’s lack of understanding of the angioarchitecture of branching, perforating arteries and the aneurysm. In addition, aggressive dissection of perforators while manipulating the aneurysm dome may lead to IOR. Temporary clipping can substantially mitigate the risk while facilitating perforator dissection. Moreover, temporary occlusion of the parent vessel significantly facilitates adequate visualization around the aneurysm neck without a need to remove brain or attempt aggressive fixed retraction.
The management of an IOR at this stage relies on a clear anatomical understanding and complete dissection of the vascular structures surrounding the aneurysm. Ideally, this dissection is accomplished from proximal to distal along the arterial tree to expose the aneurysm neck as well as the perforating and branching arteries. At this point, the aneurysm can be permanently clipped.
If the entire distal neck is not visible and clip closure does not stop the bleeding, the clip blades are either too short, not completely collapsing the neck, or there is a tear at the aneurysm neck. Therefore, temporary clips should be reapplied to allow further inspection. With proximal control in place, bleeding can generally be easily controlled with a piece of cotton and suction tip on the bleeding point.
Intraoperative Rupture of an ACoA Aneurysm Caused by the Loss of Temporary Proximal Parent Vessel Occlusion
IOR during Clip Application
At the moment the clip is applied to the aneurysm neck, IOR can occur for several reasons. A tear can occur at the neck or the sac by the tips of the blades if the surgeon has not sufficiently dissected the neck and attempts a “blind” clipping. This event can also occur when the surgeon uses the tips of the clip blades to complete dissection along the neck.
Figure 1: If the clip blades are improperly sized, the blood enters the aneurysm at a higher pressure and leads to hemodynamic turbulence within the sac, causing an IOR. Generally, the neck ovalizes and broadens upon clip application; it is not uncommon to find that the clip is too short.
Intraoperative Rupture of a Small ACoA Aneurysm due to Clip Misplacement
Figure 2: In addition to improper clip size and placement, partial closure of the clip blades can be caused by atherosclerosis at the neck and/or perpendicular rather than parallel (to the parent vessel) clip application. This technical error most commonly occurs for PCoA aneurysms.
Figure 3: Incomplete closure of the atherosclerotic neck can cause IOR. In this sketch, the distal atheroma prevents approximation of the clip blades. Placement of a second tandem clip short of the atheroma can collapse the neck. If the atheroma is at the proximal neck, a second fenestrated tandem clip is appropriate to close the distal neck.
If clip blade closure reveals a modest amount of bleeding, the operator should examine the blades to ensure that they span the entire neck of the aneurysm. If the clip is across the entire neck, complete clip blade closure should be questioned. Angled, bayoneted, and L-shaped clips have lower closing pressures than straight clips.
Figure 4: Most IORs occur from the aneurysm dome. The most dangerous situation is a tear at the aneurysm neck. This can occur because of a neck fracture at the level of an atheroma. Alternatively, the tips of the blades can penetrate the neck during blind clipping.
In these cases, attempts to place a clip more proximally at the neck can result in narrowing or occlusion of the parent vessel. Suturing to repair the neck is impossible and leads to further tearing. A more tenable option is the Sundt-Kees clip graft. This device can be used to reconstruct the vessel lumen. Unfortunately, this type of clip can be difficult to maneuver, and matching the size imperfectly will occlude perforators or adjacent branches. The cotton-clipping technique is effective.
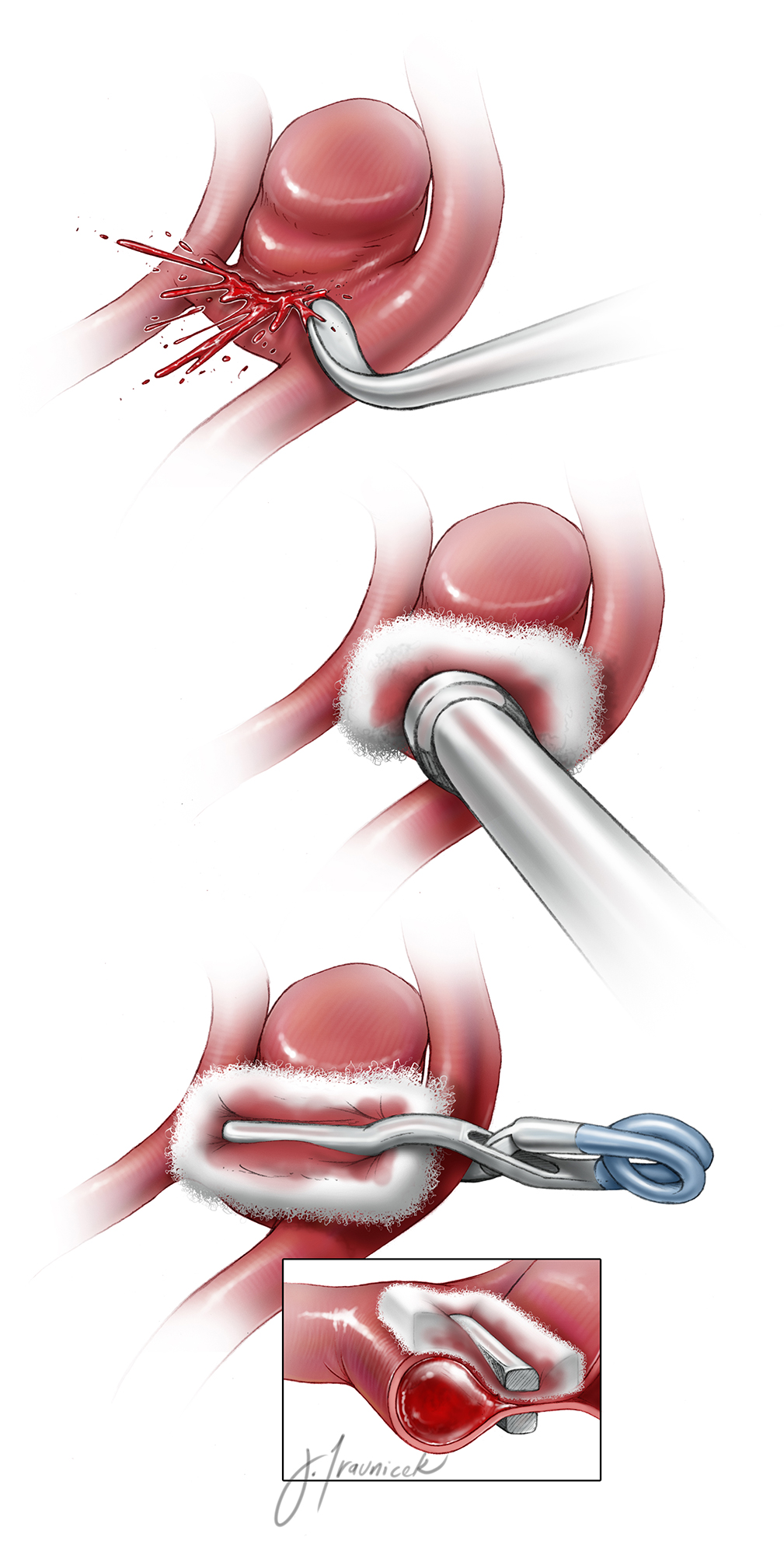
Figure 5: Tears at the aneurysm neck are controlled using the cotton-clipping technique. The surgeon covers the bleeding site with a small piece of cotton. A clip is then placed across the cotton, just above the tear, allowing the cotton to act as a bolster to seal the tear without compromising the lumen of the parent vessel.
Figure 6: Details of the cotton-clipping technique for an anterior communicating artery (ACoA) aneurysm are illustrated. Blind dissection with the dissector/clip blades or the presence of calcification or atherosclerosis at the neck may lead to a neck tear or fracture, respectively. Two large bore suctions control the overwhelming bleeding while exposure is expanded. Please see the following images for the next steps.
Figure 7: Closure of the bleeding site using a clip may be possible after temporary occlusion of the feeding vessels.
Figure 8: If primary clipping is not possible because the tear is too close to the neck, I cover the bleeding site with a small piece of cotton while using the suction tip on the cotton to keep the operative field clear of blood. A clip is then placed across the cotton, just above the tear, allowing the cotton to act as a bolster to seal the tear without compromising the lumen of the parent vessel.
Intraoperative Neck Tear and Cotton Clipping Technique for Treatment of a PCoA Aneurysm
Finally, in cases when no other option is available, the surgeon can trap the aneurysm by occluding the damaged segment of the feeding vessel with permanent clips. Although this method successfully excludes the aneurysm, it is associated with a high risk of ischemic complications. If poor collateral circulation is suspected, an extracranial to intracranial (EC-IC) or intracranial to intracranial (IC-IC) bypass is necessary.
Following is a review of the relevant technical nuances for avoidance and management of IOR among the most common surgically treated aneurysm subtypes.
Technical Nuances for Specific Aneurysm Subtypes
Anterior Communicating Artery Aneurysms
The corresponding complex regional vascular anatomy and its frequent variations (including rotation of the ACoA complex) may disorient the surgeon. Due to the presence of numerous adjacent branching and perforating arteries, including bilateral A2s and hypothalamic perforators, elaborate dissection of the aneurysm neck or dome is often necessary.
These high-risk dissection maneuvers increase the risk of IOR among ACoA aneurysms. An in-depth understanding of the aneurysm neck morphology in relationship to the dominant A1 is important for accurate clip application and avoidance of suboptimal clipping.
Partial clipping due to inadequate neck visualization, especially in the case of superior- and posterior-pointing aneurysms, can be problematic. Inferior-pointing aneurysms may interfere with securing proximal control on the contralateral A1. Temporary occlusion is especially helpful in deflating the aneurysm sac and allowing accurate clip application while maneuvering the clip blades along numerous important adjacent branches and minimizing the use of fixed retraction.
The use of straight fenestrated (ipsilateral A2 within the fenestration) clips for anterior- and superior-pointing aneurysms often leads to best results. The most common cause of IOR is relatively blind placement of the clip blades because the surgeon has not fully understood the relationship of the distal neck to the ACoA complex and contralateral A2 branches.
Blind dissection of the neck using the clip blades may lead to large tears at the neck. Small aneurysms can be troublesome since generous exposure of their neck often requires some mobilization of their dome. Removal of the gyrus rectus should be limited to the medial pial membranes until adequate proximal exposure is secured. Ultimately, a clear understanding of the regional vascular anatomy based on preoperative angiography minimizes complications.
Middle Cerebral Artery Aneurysms
Wide opening of the Sylvian fissure offers an ample amount of space to manipulate the MCA vascular tree for accurate clip application of MCA bifurcation aneurysms. However, the common occurrence of atherosclerosis and calcification at the neck of these aneurysms can interfere with complete clip blade closure. Significant intrasylvian blood can also cause the surgeon to wander and mistakenly expose the dome without proximal control.
Most IORs are easily managed using a piece of cotton over the bleeding point because the available space and superficial level of dissection readily allows microsurgical manipulation in contradistinction to the limited space afforded during exposure of ACoA aneurysms.
One of the most common causes of IOR is manipulation of the adherent en passage vessels attached to the aneurysm dome and subsequent penetration of the dome. Temporary M1 clipping provides the safest opportunity to dissect away the en passage vessel. Low flow bleeding in the case of an inadvertent sac penetration can be controlled via a small piece of cotton at the dissection site over the dome while finalizing permanent clip application.
Posterior Communicating Artery Aneurysms
Due to the relative high flow of blood within the parent carotid artery, this aneurysm subgroup leads to the most dramatic IORs. Clip application perpendicular to the carotid artery is often the most likely cause of IOR (see Figure 2). Because of the PCoA aneurysm’s thick walls, perpendicular clip application may lead to incomplete closure of the blades and intrasaccular hemodynamic turbulence, leading to IOR.
Furthermore, perpendicular clipping most often underestimates (especially in the case of large aneurysms) the size of the neck and leads to oblique partial clipping across the neck. Overzealous dissection of adherent anterior choroidal arteries by mobilizing the dome without temporary clip ligation of ICA may also cause IOR.
For these reasons, straight or angled fenestrated clips (ICA within the fenestration) provide best results by collapsing the neck parallel to the axis of the carotid artery. Because of the presence of fenestration within the clip, aggressive dissection of adherent vessels, including the anterior choroidal arteries, is often not mandatory.
Posterior Inferior Cerebellar Artery Aneurysms
Forceful cerebellar retraction should be avoided during surgery of the distal posterior inferior cerebellar artery (PICA) aneurysms attached to the tonsils. Anterior-pointing, more proximal aneurysms may adhere to the dura of the clivus; their manipulation leads to a tear at the fundus.
Because of the small diameter of the PICA, a tear at the aneurysm neck can significantly jeopardize the patency of this artery. The cotton-clipping technique described above can salvage the artery in this situation. Similarly, clip application perpendicular to the PICA may lead to either parent vessel occlusion or partial clipping.
Pearls and Pitfalls
The most common causes of IOR before clip application are:
- Use of indiscriminate blunt dissection and aggressive brain retraction
- Blind dissection around the aneurysm using a blunt probe and the surgeon’s inability to identify the correct vascular anatomy around the aneurysm.
- Blind insertion of the clip blades along the aneurysm neck without adequate visualization. In other words, the tips of the clip blades are expected to complete the dissection. In the presence of a pulsatile sac, the nervous operator wants to avoid IOR and places the permanent clip prematurely.
- Aggressive aneurysm manipulation—fighting against the “high-turgid” aneurysm—without temporary parent artery occlusion.
- Incomplete temporary parent vessel occlusion due to inadequate placement of the temporary clip across the parent artery or the presence of arteriosclerotic plaque prohibiting closure of the temporary clip blades.
Management
- Careful confirmation of regional angioanatomy will allow the surgeon to dissect proximal to distal along the arterial tree, reaching the aneurysm prepared.
- Temporary occlusion of the parent vessel facilitates adequate dissection and visualization around the entire breadth of the neck and more accurate permanent clip application.
- Following temporary clip placement, relaxation of the aneurysm should be verified (by gentle nudging of the aneurysm wall) before aneurysm manipulation is contemplated.
- If the entire distal neck is not visible and clip closure does not stop bleeding, a tear at the aneurysm neck is suspected and temporary clipping and thorough inspection is necessary.
The most common causes of IOR during clip application are:
- Partial clipping leads to increased hemodynamic pressure within the aneurysm sac and rupture.
- The aneurysm dome may be adherent to the surrounding brain. Traction on the dome during clip placement may prevent complete clip blade closure.
- Atherosclerotic plaque at the aneurysm neck leads to partial clipping and IOR.
- Clip application parallel to the long axis of the parent vessel is imperative when anatomically possible, especially for aneurysms originating directly from the internal carotid artery. Perpendicular clipping may lead to inadequate clip blades closure and delayed clip displacement.
Management
- Thorough inspection and understanding of the aneurysm anatomy is critical before clip application.
- For large adherent aneurysms, careful dissection of the midbody and dome of the aneurysm may be needed to prevent excessive traction on the aneurysm dome during clip closure.
- Tandem clipping should be considered early to avoid partial clip closure among aneurysms with wide atherosclerotic necks.
Final Thoughts
During IOR, the surgeon may start with two suctions to clear the field and identify the site of the leak and then keep the field clear using only a single suction over the exact site of the hemorrhage. Local circulatory arrest via proximal and distal temporary occlusion of the parent vessel(s) and administration of cerebral protectant, while maintaining normotension, will allow continuation of sharp dissection. Exploration of the exact site of the bleeding relative to the aneurysm neck, parent vessel, and important neighboring perforators can then be completed.
If closure of the clip blades reveals a modest amount of bleeding, the operator should examine the blades to ensure that they encompass the entire aneurysm neck. If the clip is across the entire neck, inadequate clip closing pressure caused by undetected atherosclerosis or calcification should be considered.
A tandem clipping technique using both a fenestrated and straight clip may be necessary to ensure complete obliteration of the aneurysm. Plaque near the hinge of the clip may prevent distal clip closure. In such circumstances, a fenestrated clip may be added to close off the distal neck.
If the initial clip is deemed too short, a second, longer clip may be applied in tandem with the first one; the first clip is then removed and the second clip moved proximally across the neck. Excessive bleeding after closure of the clip blades raises the suspicion of a neck tear, and the cotton-clipping technique should be considered along with local circulatory arrest.
Personal Reflections
IOR is a preventable complication that can be devastating if the surgeon does not understand the causes and management options available. Accurate knowledge of the anatomy of the aneurysm and surrounding vasculature is the keystone to both prevention and treatment of IOR.
Most importantly, the surgeon must not rush to clip blindly in an effort to stop the hemorrhage. It is usually not the rupture that causes death and disability, but the surgeon’s subsequent actions that can be the difference between a good or poor outcome. Ultimately, major complications related to IOR are caused by the surgeon’s premature reaction while placing a permanent clip in the event of torrential bleeding without adequate visualization, leading to vascular and cranial nerve injuries.
Contributors: Albert J. Schuette, MD, and Daniel L. Barrow, MD
Note: This work has been modified and was originally published as: Schuette AJ, Barrow DL, Cohen-Gadol AA. Strategies to minimize complications during intraoperative aneurysmal hemorrhage: A personal experience. World Neurosurg 2015; 83(4)620-626.
References
Batjer H, Samson D. Intraoperative aneurysmal rupture: Incidence, outcome, and suggestions for surgical management. Neurosurgery. 1986;18(6):701-707.
Fridriksson S, Saveland H, Jakobsson KE, et al. Intraoperative complications in aneurysm surgery: A prospective national study. J Neurosurg. 2002;96(3):515-522.
Giannotta SL, Oppenheimer JH, Levy ML, Zelman V. Management of intraoperative rupture of aneurysm without hypotension. Neurosurgery. 1991;28(4):531-535; discussion 535-536.
Leipzig TJ, Morgan J, Horner TG, Payner T, Redelman K, Johnson CS. Analysis of intraoperative rupture in the surgical treatment of 1694 saccular aneurysms. Neurosurgery. 2005;56(3):455-468; discussion 455-468.
Wong JM, Ziewacz JE, Ho AL, et al. Patterns in neurosurgical adverse events: Open cerebrovascular neurosurgery. Neurosurg Focus. 2012;33(5):E15.
Lawton MT, Du R. Effect of the neurosurgeon's surgical experience on outcomes from intraoperative aneurysmal rupture. Neurosurgery. 2005;57(1):9-15; discussion 19-15.
Sandalcioglu IE, Schoch B, Regel JP, et al. Does intraoperative aneurysm rupture influence outcome? Analysis of 169 patients. Clin Neurol Neurosurg. 2004;106(2):88-92.
Schramm J, Cedzich C. Outcome and management of intraoperative aneurysm rupture. Surg Neurol. 1993;40(1):26-30.
Elijovich L, Higashida RT, Lawton MT, Duckwiler G, Giannotta S, Johnston SC. Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: The CARAT study. Stroke. 2008;39(5):1501-1506.
Wong JM, Ziewacz JE, Panchmatia JR, et al. Patterns in neurosurgical adverse events: Endovascular neurosurgery. Neurosurg Focus. 2012;33(5):E14.
Ogawa A, Sato H, Sakurai Y, Yoshimoto T. Limitation of temporary vascular occlusion during aneurysm surgery. Study by intraoperative monitoring of cortical blood flow. Surg Neurol. 1991;36(6):453-457.
Horiuchi T, Rahmah NN, Yanagawa T, Hongo K. Revisit of aneurysm clip closing forces: Comparison of titanium versus cobalt alloy clip. Neurosurg Rev. 2013;36(1):133-138.
Barrow DL, Spetzler RF. Cotton-clipping technique to repair intraoperative aneurysm neck tear: A technical note. Neurosurgery. 2011;68(2 Suppl Operative):294-299; discussion 299.
Please login to post a comment.